
Public health expert Huang Yanzhong: “rapid peak” can cause unnecessary serious illness and death
On December 25, the National Health Commission issued a note: From now on, no more daily outbreak information will be released, and relevant outbreak information will be released by the China Center for Disease Control and Prevention for reference and research purposes.
With 2022 coming to a close, most of the various new crown prevention and control measures that have been strictly enforced for three years will become history.
Many medical institutions in Shanghai, Xi’an, and Tianjin no longer check for negative nucleic acid certificates for outpatients. In Suzhou, the “nucleic acid sampling booth” has been changed to a “fever clinic”. Trip codes and health codes are retiring from the historical stage. Zhejiang and Chongqing have also proposed that people with mild, asymptomatic infections can go to work.
The policy shift is accompanied by a massive wave of infections in many places. At the same time, various predictions of peak epidemics are appearing on the Internet for various locations.
The new epidemic seems to be on its “last leg”. What should we do to make this journey more stable, less costly and less painful? In this regard, Huang Yanzhong, senior fellow for global health at the Council on Foreign Relations and professor at the School of Foreign Affairs and International Relations and director of the Center for Global Health Studies at Western Eastern University, gave his views to the medical community.

Nighttime emergency patients wait in line for treatment at the fever clinic at Beijing Anzhen Hospital.
The medical community: At present, the epidemic is still developing rapidly in many places, and medical resources are tight in some areas. Based on this, will the peak of the epidemic be more severe in China than in other countries or regions?
Huang Yanzhong: That’s not necessarily true. The virulence of Omicron has dropped to a low point and the disease and death rate is very low. Although the transmission force is at a high point, as long as the peak curve of medical resource crowding is not exactly the same across regions, for example, if place A peaks on January 1, 2023, and place B peaks in February, human and material resources can be mobilized nationwide to assist a specific region or several regions. This is like a fire-fighting team that goes to the next place after the peak in this place is suppressed. A similar approach has been used previously in the implementation of the zeroing policy.
The rapid spread of Omnicron in China is due to several factors. These include the fact that few people had a history of past infections before the liberalization, that earlier vaccinations were less effective in preventing omicron infection, and that most people have had more than six months since their three doses. This means that not only has the population not developed natural immunity, but the immunity developed by the vaccine is also weaker.
Therefore, it is very important to now emphasize the importance of getting the 4th dose and using heterologous sequential vaccination as much as possible. However, based on prior experience, it will take almost four or five months to complete a round of vaccination. By that time, the wave of the epidemic will be almost over.
MB: What other measures do we need to take at this point to help mitigate the pressure caused by the sudden liberalization?
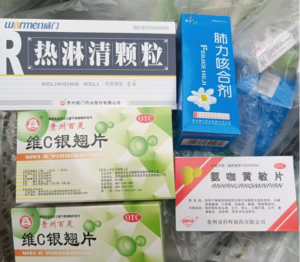
Huang Yanzhong: There are many more things to do. For example, there could be some new crown medication guidelines coming out from the national level to tell the public about reasonable drug combinations, contraindications to medication, etc. Now there are few authoritative and credible platforms that are doing these science popularization. It is particularly important that the public trusts the information released at the national level, especially for the rural population where information channels are relatively homogeneous.
In addition, outbreaks cannot be stopped, so what can be done is to keep the peak infection down to a level that the health care system can handle, through triage measures and other means that can have short-term effects. As long as multiple sites do not reach peak infection at the same time, resources and personnel can be mobilized.
It is important to note that the current announcement of the number of new infections, etc., does not address hospitalization rates, critical care bed occupancy rates, etc. These are important indicators of the actual infection situation. There are reports that the number of critical care beds per 100,000 people in China has reached 10, which is close to the level of developed countries. In terms of hardware, it may be possible to significantly increase the number of critical care beds in the short term by stepping up investment, but the hard part is staff training; it takes at least 3-5 years for a critical care physician to practice independently. It should also be taken into account that in addition to new crowns, China has a large number of critically ill patients caused by cancer and cardiovascular disease that need to use specialty ICUs. if all specialty intensive care beds are used to treat new crown patients, then cancer and cardiovascular patients cannot be hospitalized for timely treatment, which will bring secondary disasters.
Medical: If the number of infections is rising particularly fast in certain places, is it necessary to take stricter localized preventive measures?
Huang Yanzhong: Now there is an argument such as restarting the square cabin into a sub-determined hospital for initial diagnosis, triage, and admission of those who are not in a position to be isolated at home. This is a better approach. But the question is whether the public is willing to cooperate, especially considering the poor conditions of many local square cabin.
In addition, there is a tendency to note that it is hoped that the more people infected the better, the sooner the peak, the better, and strive to have 80%-90% of people infected around the Spring Festival, it is equivalent to the whole country vaccinated. That way there is a guarantee that work will resume and production will resume when the spring is in full swing. This idea runs counter to the idea of depressing the peak and is very risky. It is actually similar to the Swedish idea of “herd immunization”, except that the latter emphasizes the protection of risk groups such as the elderly.
The Swedish approach has been shown to be unworkable. Under the “rapid peak” approach, the elderly are not adequately protected, which can lead to unnecessary serious illness and death. Moreover, the spread of the virus in unvaccinated populations may lead to the emergence of new strains.
In addition, natural infection does not create lifelong immunity, which usually lasts for about 3 months, after which there is a possibility of repeat infection. So the claim of herd immunity is not realistic. This is for the same reason that herd immunity to influenza cannot be developed.
Patients attending fever clinics at medical institutions in Dongguan, Guangdong Province, have increased significantly recently.

Medical: In early December, you wrote an article predicting the number of infections and the average number of new serious illnesses per day for the current round of the epidemic in China, do you still uphold the predictions you made then today?
Huang Yanzhong: If you read the original article, you will know that it was not actually my prediction, but the research and analysis data I quoted. All predictions about the development of the epidemic are based on certain assumptions and are flawed and debatable. Some may be more credible than others, while others are not, and some are even far from reality.
The U.S. Institute for Health Metrics and Evaluation (IHME) model suggests that China’s sudden liberalization of strict restrictions on new crown outbreaks could lead to a surge in cases. New cases would peak around April 1, 2023, when about one-third of the Chinese population would be infected and result in 1 million deaths from neo-crown in 2023. According to the IHME blurb, the relevant projections use official Chinese vaccination information (timing unknown), as well as provincial response assumptions in the event of rising infection rates, and use a large amount of data from the Hong Kong region.
A recent preprint from the University of Hong Kong predicts that China’s liberalization of the new crown vaccination restrictions between December 2022 and January 2023, along with the reopening of all provinces, will result in 684 deaths per million people during that period. That works out to a total of nearly 1 million. The article is subject to peer review.
The data I cited at the time came from a Bloomberg study. It suggested that if 1/4 of the Chinese population were to become infected within the first 6 months of policy liberalization, China could have 363 million new infections, about 620,000 deaths, and 32,000 admissions to intensive care units per day.
I would like to highlight the very high rate of readmissions described in this study. However, if China could stagger the infections, there would not be so many beds needed at the same time, there would not necessarily be a run on medical resources, and there would not be so many deaths.
Medical profession: Is there an “ideal” time to liberalize?
Huang Yanzhong: The academic community has different views on this issue. Wu Zunyou, chief epidemiologist at the CDC, said in his keynote speech at the Annual Finance Conference on December 17 that the current moment is “the best point” because it is “the lowest number of reported deaths per week in three years. It’s also the lowest number of reported deaths per week in three years and the lowest number of reported deaths per week in three consecutive weeks in its three-year history.
But in fact, from April to November of this year, when Shanghai closed its control management, the death rate of new infections in China was essentially zero. Now liberalization has the added problem of facing the flu season, when two viruses with similar symptoms may strike at the same time, putting even more pressure on the healthcare system.
In fact, the timing of optimizing prevention and control is a very unidirectional prediction criterion, as assessed by the disease and death rate. In my opinion, the factors to be considered in the liberalization of prevention and control policies include, first, the characteristics of the virus itself. Omicron has fallen to very low mortality levels earlier this year, which is a favorable factor that can be liberalized. Second, the secondary disasters caused by the dynamic clearance measures to the economy and society, including the negative impact of long-term strict closure and control management on people’s mental psychology. This situation should also be considered for liberalization. Third, physical isolation and other measures are difficult to resist the rapid spread of the virus, and the cost of prevention and control is getting bigger and less effective. Fourth, if a roadmap is planned and prepared for liberalization, the negative impact can be minimized.
In addition to the timing of liberalization, the manner, process and supporting measures are equally important. I am in favor of gradual and prepared liberalization.
Medical profession; in order to achieve what you call “progressive adjustment”, what preparations need to be made?
Huang Yanzhong: Gradual adjustment needs a roadmap, that is, to what point and how much to liberalize. In Australia, the degree of liberalization is linked to the vaccination rate. Singapore is based on the development of the epidemic, to plan when to dine-in, adjust the number of people in the party, etc.. The practices that countries have already undertaken can tell us which paths are better and which practices are better.
Progressive adjustment is not a reactive process, and even if there is a roadmap, it depends on whether the measures are implemented quickly or whether the virus is running fast. The current rate of spread of the new coronavirus in China is probably the fastest in the world, and it is something that no other country or region has ever experienced. For example, the United States reached 25% of the population infected with Omicron in 6 months. There are predictions that Beijing is expected to reach a high point of infection in mid-January 2023, which may have already been achieved under the current scenario.
There has been much discussion online about the preparations for liberalization. In general, they include strengthening public medical construction and increasing the number of critical care beds; stockpiling more drugs; upgrading the number of community hospitals and fever clinics; guiding intra- and inter-hospital triage and streamlining treatment procedures; providing psychological guidance and operational training for medical staff to instruct them to protect themselves; and planning a rotation system for physicians to cope with staff shortages after an infection.
It was also suggested that the experience of Japan and the United States could be combined with the distribution of anti-new crown drugs at the government level to ease the pressure of drug shortage. Chinese people have the habit of hoarding things. Originally, one box of medicine was enough for a family to share, but now everyone hoards it, and once they hoard dozens of tablets, there may be a shortage of drugs at the social level. Many people go to the hospital, not to see a doctor, but to get medicine. This makes it difficult for people who really need medical attention and medicine to get effective treatment.
In terms of centralized management of epidemic prevention materials, the Japanese government gives the people a quick antigen screening kit, and when people call the authorities after testing themselves positive, the government sends the new crown drug free of charge. In this way, people have a willingness to report if they have a positive test, and positive data can be collected at the national level, and the statistics are reliable. At the same time, the orderly distribution of supplies makes it less likely to cause a run on medical resources and prevents the spread of infections caused by the process of seeking medical care. Companies will also be able to quickly start up and produce more drugs based on actual demand.
China has always had the advantage of concentrating its efforts to do great things, and is fully capable of doing this kind of resource coordination and management.
Medical: With 1 month to go before the Chinese New Year, what will be the likely situation if allowed to return home for the New Year?
Huang Yanzhong: Mr. Wu Zunyou said at the annual financial conference that China will face “one peak and three waves”, of which the second wave will be during the Spring Festival in 2023. To be precise, there will be three epidemic prevention peaks in the next three months. It is not unprecedented in other countries to have such a peak followed by another wave, but it is less common to experience three waves in three months.
From a socio-psychological point of view, it is unlikely that China will promote the “New Year in Place” again this year. Then, with more than 200 million people on the road, the Omicron strain could spread from the current urban areas to the rural areas on its way back home. Different strains could also mix across the country.
On the one hand, this will pose a huge challenge to the rural health care system, treatment capacity, and prevention barriers. The previous epidemic prevention policy deployment stated that township health centers must have fever clinics, and coverage will be increased from 45% to 90% by the end of March 2023. This time requirement may be too late to respond to the wave of the epidemic.
On the other hand, even if township health centers have fever clinics, it is hard to say whether the public will go there because the level of medical services cannot keep up. As it stands now, the treatment in many places at the rural grassroots level is an IV drip, which is not a standard treatment. Some rural populations, unable to get effective treatment locally, return to the cities, creating pressure for access to care.
The situation is stronger than the people, and plans cannot catch up with changes. Some measures, even if done now, may not be able to keep up with the speed of the virus’ spread. This is what we call path-dependent selection.

Average Rating