
Immunoglobulin against the new crown is not yet on the market, what is the mad rush?
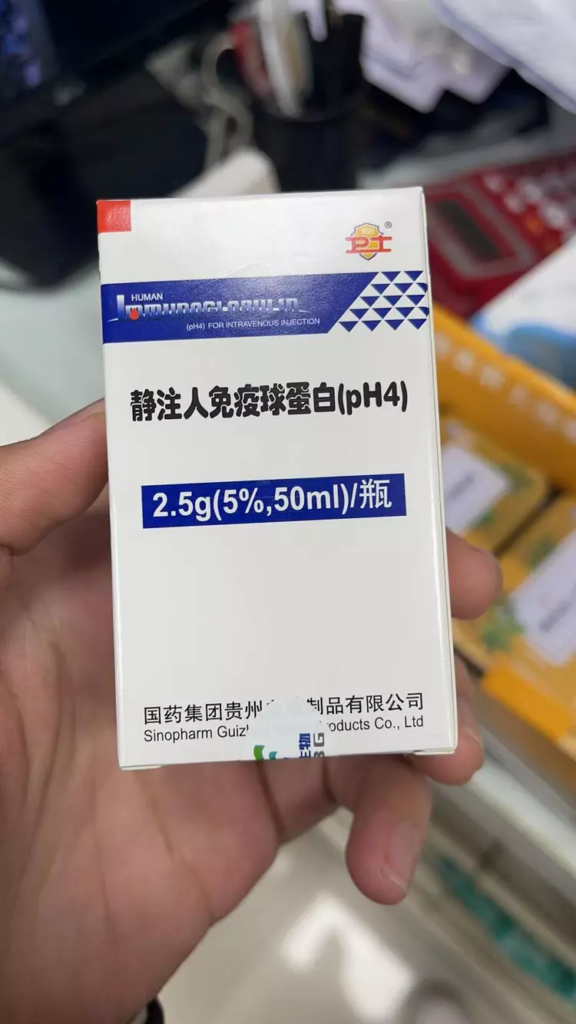
Following drugs such as Lianhua Qingdian, imported antiviral drugs, and montelukast, in the past few days, sedative human immunoglobulin is becoming another target to be snapped up in the new crown pandemic. According to media reports, its price has risen from the normal several hundred yuan a piece to more than two thousand dollars.
The intravenous human immunoglobulin, referred to as “Jing C” or “gammaglobulin”, is used to treat primary immunoglobulin deficiency, secondary immunoglobulin deficiency diseases, autoimmune diseases (such as Kawasaki disease in children, primary thrombocytopenic purpura) etc.
On January 4, a pediatrician posted on social media, “Now Kawasaki disease patients, you can’t find immunoglobulin.” Kawasaki disease is an acute febrile rash childhood disease with systemic vasculitis as the main lesion, which requires immunoglobulin treatment after the onset of the disease.
A respiratory physician at China-Japan Friendship Hospital said bluntly in an interview with China Newsweek, “There is no international evidence of evidence-based medicine that immunoglobulin (which is being madly sought after) can treat people with new crown infections. So we are not recommending its use.”
On Jan. 5, the 10th edition of the treatment protocol for neo-coronavirus infection, released by the National Health Commission in conjunction with the National Bureau of Chinese Medicine, mentions that intravenous COVID-19 human immunoglobulin can be used early in the course of the disease in patients with high risk factors for severe disease, high viral load and rapid disease progression. However, this immunoglobulin is not the ordinary intravenous human immunoglobulin that people currently buy.

Immune Globulin
The wildly sought-after gammaglobulin is not for the new crown
Xu Pehong and others from the Department of Pharmacy, Ruijin Hospital, Shanghai Jiaotong University School of Medicine, published a paper in 2020, “Analysis of the Current Situation and Development Trend of Blood Products Production and Use in China,” pointing out that human immunoglobulin accounts for 14.53% of the domestic blood products market, and other blood products drugs include human albumin and recombinant human thrombopoietin.
Intravenous human immunoglobulin (IVIG) is an immune substance produced by the body’s immune system after being stimulated by antigens. Immunoglobulins can be divided into various subclasses such as IgA, IgG, IgM, etc. Immunoglobulins used for medicinal purposes are mainly IgG.
Gammaglobulin is mainly used clinically to enhance immunity and treat primary immunoglobulin deficiency, secondary immunoglobulin deficiency and autoimmune diseases. In the treatment of hypogammaglobulinemia, antibody deficiency diseases, or other immunodeficiency states, Jing C can exert an anti-inflammatory effect by providing passive immunity, i.e., sufficient concentrations of antibodies against a variety of pathogens.
“Gammaglobulin is rarely used by us in the clinical treatment of patients with neocoronary disease, except in the treatment of a category of pediatric disease called multisystemic inflammatory syndrome (MIS-C), where this drug is supported by clinical data and is included in the appropriate guidelines.” Lei Gao, president of the North American Chinese Physicians Coalition and an expert member of the American College of Cardiology (FACC), said in an interview with
In both the ninth edition, released in March 2022, and the tenth edition, which has just been updated, the “antiviral treatment” of the new crown includes five therapies: antiviral drugs, monoclonal antibodies, intravenous COVID-19 human immunoglobulin, and recovery plasma for recovered patients.
In the case of COVID-19 human immunoglobulin, both protocols state that it can be used early in the course of the disease in patients with high risk factors, high viral load, and rapid disease progression. The tenth edition of the treatment protocol states that the dose used is 100mg/kg for light duty, 200mg/kg for medium duty and 400mg/kg for heavy duty by intravenous infusion, which can be reinfused the next day for a total of no more than five times depending on how the patient’s condition improves.
“The intravenous human immunoglobulin that people are currently snapping up is not a New Crown patient-specific treatment drug; COVID-19 human immunoglobulin is the New Crown pneumonia-specific treatment drug.” Li Meng, a pharmacist in charge of the Department of Pharmacy at Tongji Hospital of Huazhong University of Science and Technology, pointed out. In addition to intravenous COVID-19 human immune globulin, there are many other immune globulins that are specific, for example, hepatitis B human immune globulin, rabies human immune globulin, and tetanus human immune globulin. In other words, COVID-19 human immunoglobulin is only one of the “Jing C”.
In early September 2021, Sinopharm announced that Titan Biologicals, a blood products company, had received approval from the State Drug Administration to conduct clinical trials on COVID-19 human immune globulin. According to Titan Bio, COVID-19 human immunoglobulin is a new class I drug for therapeutic biologics, and is the world’s first drug for the specific treatment of neocrown pneumonia prepared from plasma after immunization with inactivated neocrown vaccine. In other words, COVID-19 Human Immunoglobulin is purified from the plasma of people who have recovered from New Crown pneumonia to produce a globulin containing antibodies from the recovered people.
According to the report, Titan Bio is the only company specializing in blood products under China Bio. The company announced at the time that the static injection of COVID-19 human immunoglobulin was an original product of Titan Bio, with no similar product listed at home or abroad, and that the product had been invested in research and development for RMB 29,772,900.
In February 2022, Titan Biologicals released information that its intravenous COVID-19 human immunoglobulin has now completed clinical ethics review, clinical drug clearance, preclinical enrollment and other preparatory work in accordance with the requirements of drug clinical trials, and has recently conducted phase II clinical trials in the UAE. However, according to the reporter’s inquiry, there is no news about the completion of clinical trials or the listing of the drug as of now.
China Newsweek consulted with the chiefs of critical care and infection departments of several hospitals in Beijing and Guangzhou, all of whom said that the immunoglobulin for the new crown was not available and that they had not used it themselves.
Photo
Gammaglobulin for severe neocon disease: lack of evidence to support it
Gao Lei, president of the North American Chinese Physicians Coalition and an expert member of the American College of Cardiology (FACC), told China Newsweek that recently, the North American Chinese Physicians Coalition has organized a number of online meetings involving both U.S. and Chinese physicians on the experience and latest advances in the treatment of anti-epidemic disease in the United States. “A very important lesson is that the protocols used in treatment must be supported by clinical data, for example, regarding the controversial hormone therapy, which has accumulated more and more evidence of effectiveness among new crown treatments.” He said.
However, sedated human immunoglobulin for neocon therapy falls into the category of drugs that are not supported by the evidence. The transition from severe to critical illness in patients with neocon can be associated with an excessive immune response. As a result, anti-inflammatory drugs, including corticosteroids, have been reintroduced for the treatment of critically ill patients with neocolonial infections. However, the clinical efficacy and safety of gammaglobulin, which is also an anti-inflammatory class of drugs, is controversial in the treatment of neocon.
Recently, different hospitals have issued different treatment reference guidelines with different attitudes toward immunoglobulins. For example, the diagnosis and treatment guidelines of West China Hospital recommend gammaglobulin. The Department of Respiratory Medicine at Tsinghua Changgeng in Beijing suggests that for patients with heavy or critical neocoronavirus pneumonia, gammaglobulin and glucocorticoid hormone are recommended to be used together or alone; in addition, neocoronavirus-specific immunoglobulin or monoclonal immunoglobulin can also be applied for treatment.
Currently, the World Health Organization, the CDC and other agencies do not include gammaglobulin in the treatment regimen for neointima. The “Expert opinion on the clinical management of severe infection due to Neovirus caused by Omicron” recently published by Dr. Zhan Qingyuan, chief physician of the Department of Respiratory and Critical Care Medicine at the Respiratory Center of China-Japan Friendship Hospital, clearly states that the use of gammaglobulin and recovery plasma is not recommended for treatment.
In July 2022, a study published in Expert Review of Antiviral Therapy by Taiwanese physicians Lai Chi-ching et al. in a meta-analysis of 6 randomized controlled trials of intravenous human immunoglobulin in 472 patients showed that gammaglobulin did not improve clinical outcomes in hospitalized patients with neocoronavirus pneumonia in terms of mortality, mechanical ventilation, need for ICU admission, and length of stay. improve clinical outcomes.
Similarly, a paper published in February 2022 in The Lancet – Respiratory Medicine reported on a multicenter, double-blind, placebo-controlled phase III clinical trial conducted in France. The results showed that in patients with moderate-to-severe neocoronary who required invasive mechanical ventilation for ARDS (acute respiratory distress syndrome), sedation of immunoglobulin did not improve clinical outcomes in subjects at day 28 of their evaluation. In addition, the study results showed an increased probability of serious adverse events in the study group using gammaglobulin, including mainly deep vein thrombosis and pulmonary embolism.
On January 27, 2022, a paper was published in Frontiers in Immunology by many critical care experts, including Bin Du, director of the Internal Medicine ICU at Peking Union Medical College Hospital, and Haibo Qiu, director of the Department of Critical Care Medicine at Zhongda Hospital, Southeast University School of Medicine. The article analyzed 754 ICU inpatients from 19 hospitals during the Wuhan outbreak in 2020, 392 of whom received intravenous human immunoglobulin treatment. The results did not reveal a significant correlation between the use of gammaglobulin and reduced mortality, nor was any survival benefit obtained.
Wang Guiqiang, director of the Department of Infection at Peking University First Hospital, said in an interview with CCTV earlier this January that intravenous gammaglobulin can reduce inflammatory reactions, but is only recommended for use in treating critically ill patients, saying, “Basically, it is only needed for patients entering the ICU, and it is only effective when used in specific situations such as inflammatory factor storms, and is not suitable for home use, and there is no role in preventing new crown infections, and it is not recommended to stock up at home.”
Li Meng, pharmacist in charge of the pharmacy department of Tongji Hospital of Huazhong University of Science and Technology, stressed that gammaglobulin is a blood product and its improper use can bring a lot of side effects; and the drug cannot be expanded in capacity like antipyretics, and its use should be strictly controlled during the special period when supply exceeds demand, leaving it for patients with real needs.

Infographic
Hualan Bio is a domestic enterprise engaged in the research, development, production and sales of biological products such as blood products, vaccines and recombinant proteins. In its official website, the company points out that since the raw material for the static injection of human immunoglobulin comes from human blood, although the raw plasma is screened for relevant pathogens and measures to remove and inactivate viruses are incorporated in the production process, there is still a theoretical potential risk of spreading certain known and unknown pathogens, and the pros and cons should be weighed when used clinically.
If the drug is used without authorization, an infection doctor told China Newsweek, it may bring about side effects on the nervous system, blood system side effects, and damage to the kidneys. In addition, as a blood product, human immunoglobulin is also prone to allergic reactions during infusion, which can be life-threatening in severe cases.
The National Institutes of Health, in its December 1, 2022, update of the new coronary care guidelines, wrote that gammaglobulin is not recommended for the treatment of acute COVID-19 in adults and children except in clinical trials; gammaglobulin in combination with low to moderate doses of glucocorticoids is recommended for the treatment of multisystemic inflammatory syndrome in children (MIS-C) in hospitalized patients, but routine use of gammaglobulin is not recommended monotherapy for MIS-C.
In the United States, official guidelines are regularly updated about once every six months based on the results of clinical trials, Gao Lei noted, because the evidence for drugs is constantly changing. For example, during the Delta epidemic, the U.S. also used monoclonal antibodies to treat New Crown, but after the appearance of the Omicron mutant strain, recovery plasma therapy and monoclonal antibodies were ineffective.
He suggested that relevant clinical trials could also be conducted in China to determine the efficacy of gammaglobulin, “In fact, there are enough patients with neo-crown in China now that a 30 ~50 day clinical trial can actually observe the results regarding whether gammaglobulin is effective.”
An infection physician at a large tertiary hospital has also pointed out to China Newsweek that the National Health Commission’s treatment plan should clearly state how effective it is against Omicron by giving evidence-based evidence for some treatment options for which there is no evidence or insufficient evidence, like plasma for recovering patients and monoclonal antibodies.
For the new crown-specific immunoglobulin, Gao Lei said, from the principle or theory, many drugs can be tried, but in the end, all need to be supported by clinical data, ineffective to discontinue, no need to waste medical resources; at the same time, the drugs in clinical trials should not enter the guidelines.

Average Rating