
Zhang Wenhong’s latest speech makes two appeals, saying the country has the ability to turn an outbreak into an endemic epidemic
What are the future trends of the new crown epidemic in China? How to save the lives of more vulnerable people such as the elderly? At the 2nd Guanghua Forum held yesterday, Professor Zhang Wenhong, Director of the National Center for Infectious Diseases and Director of the Infection Department of Huashan Hospital of Fudan University, gave a keynote speech. In his opinion, after China enters the first wave of mass epidemic, it will gradually enter the stage of endemic, “in sync” with the world.
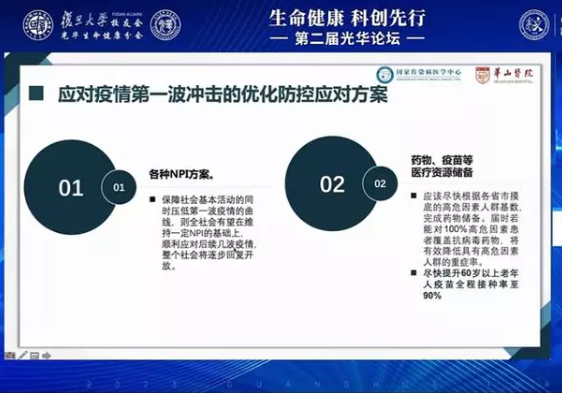
During the transition period from mass to endemic epidemics, he called for the completion of drug stockpiles as soon as possible based on the base of high-risk factors mapped by provinces and cities. “If antiviral drugs can be covered for 100% of patients with high-risk factors, it will effectively reduce the rate of serious illness in people with high-risk factors.” He also called for: increasing the full vaccination rate to 90 percent for people over 60 years of age as soon as possible.
“I believe that China has the ability to turn a new crown epidemic into an endemic.” Zhang Wenhong said. Forum moderator and Fudan University professor Lu Dairu said, “Director Zhang’s speech has strengthened everyone’s confidence in fighting the epidemic.”
File photo
Why Singapore’s “performance” against the epidemic is better than that of the United States
In his speech, Zhang Wenhong introduced that in the past 100 years, there have been five large-scale epidemics of infectious diseases around the world. In addition to the new crown, the first four were influenza, respectively, the 1918 Spanish flu, 1957-1958 Asian flu, 1968-1969 Hong Kong flu, 2009-2010 H1N1 flu.
Today, influenza has become an endemic epidemic, with only nearly 200,000 influenza-related deaths worldwide each year. Of course, this figure may be an underestimate because of the insufficient amount of influenza virus detection.
So, will the new crown also evolve from a global pandemic to an endemic? Wenhong Zhang gave an affirmative answer. In some countries, after the public has experienced the pain of a large pandemic, the number of excess deaths has now been significantly reduced. Excess deaths are the difference between the number of deaths that actually occurred in an area and the number of deaths estimated in years when no epidemic occurred, and can more accurately reflect the lethality of an infectious disease. In Singapore, for example, excess deaths have been close to 0, and the new crown disease death rate has been very low recently.
According to Wenhong Zhang, an important reason for the dramatic reduction in excess deaths in Singapore during the Omicron variant epidemic is that the vast majority of elderly people completed the 3-dose vaccination during the Delta variant epidemic.
In contrast to Singapore, omicron is highly lethal in the United States. Statistical analysis shows that the peak excess mortality caused by omicron in Americans aged 65 years and older was 163% of the delta peak. This is closely related to the lack of full vaccination coverage of older Americans. The dramatic increase in medical visits and hospitalizations of older adults has also led to a crowding out of medical resources, which further inflates excess mortality.
Fact Sheet
“Many people are concerned that the levels of antibodies produced by various vaccines are diminished, leading to breakthrough infections. So is vaccination useless?” To this question. Wenhong Zhang introduced a study he led his group to conduct last year – using single-cell sequencing technology to analyze B lymphocyte clonal amplification 3-6 months after vaccination – and found that at very low antibody levels after 6 months, B lymphocytes, especially memory B cells, were The results showed that B lymphocytes, especially memory B cells, rapidly cloned and expanded after the invasion of Omicron. This indicates that the immune cells have a strong “memory”, and even without antibodies, the virus will still trigger an immune response when it enters the body.
Preventing medical runoff by making drugs available at the grassroots level
In the optimal prevention and control response plan for the first wave of the epidemic, it is also important to have a good stockpile of drugs. At present, anti-neo-coronavirus drugs have entered a multi-pipeline competition situation, with Paxlovid (nematovir/ritonavir), Azulfidine, Monoravir, monoclonal antibodies, and intravenous COVID-19 human immunoglobulin, bringing a variety of options for clinical treatment of vulnerable populations. In addition, anti-inflammatory drugs such as tolimumab and baricitinib are also in place.
Currently, the relevant departments should complete the drug stockpile as soon as possible based on the base number of people with high-risk factors mapped by provinces and municipalities. “There should be drugs available at the grassroots level so as to prevent secondary and tertiary medical resources from being squeezed.” Zhang Wenhong said.
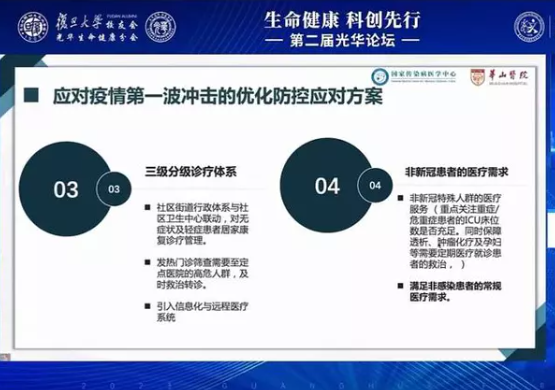
Localities should also strengthen the three-tier hierarchical diagnosis and treatment system, including: linkage of the community street administrative system with community health service centers to provide home rehabilitation treatment and management for asymptomatic and mildly ill patients; fever clinics to screen out high-risk people who need to go to designated hospitals for timely treatment and referral; and the introduction of information technology and telemedicine systems.
Zhang Wenhong said, in the “golden 72 hours” after the onset of infection, community health centers should make full use of antiviral small-molecule drugs, while oxygen therapy, traditional Chinese medicine and low-dose hormone therapy can be used. “Chinese herbal medicine will give the Chinese an additional complementary healing effect.”
File photo
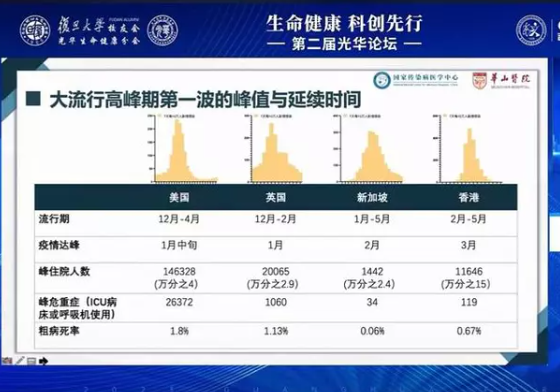
During the presentation, Zhang Wenhong cited a number of data from the United States, the United Kingdom, Singapore and Hong Kong, China, during the first wave of the new crown pandemic peak: the United States continued for five months, with a peak hospitalization of 146,328 (4 per 10,000) and a crude death rate of 1.8 percent; the United Kingdom for three months, with a peak hospitalization of 20,065 (2.9 per 10,000) and a crude death rate of 1.13 percent; and Singapore for five months, with a peak hospitalization of 1,442 ( 2.4 per 10,000) and a crude mortality rate of 0.06%; Hong Kong, China, 4 months, peak hospitalization 11,646 (15 per 10,000) and a crude mortality rate of 0.67%.
Mainland China is now also entering the first wave of the peak pandemic, and we will transition to an endemic phase as medical resources are gradually put in place. “The end result is likely to be a global convergence, just like influenza, which becomes a seasonal epidemic.” Wenhong Zhang said, “Of course, whether the new coronavirus will undergo major mutations in the future, leaving the population lacking preexisting immunity, will require close monitoring by scientists in the future.”


Average Rating